A subscription to JoVE is required to view this content. Sign in or start your free trial.
Method Article
Growing Desmoplastic Three-Dimensional Pancreatic Cancer Spheroids from Co-Culture
In This Article
Summary
Pancreatic cancer remains one of the toughest cancers to treat. Therefore, it is critical that pre-clinical models evaluating treatment efficacy are reproducible and clinically relevant. This protocol describes a simple co-culture procedure to generate reproducible, clinically relevant desmoplastic spheroids.
Abstract
Pancreatic ductal adenocarcinoma (PDAC) is one of the deadliest cancers with a 5-year survival rate of <12%. The biggest barrier to therapy is the dense desmoplastic extracellular matrix (ECM) that surrounds the tumor and reduces vascularization, generally termed desmoplasia. A variety of drug combinations and formulations have been tested to treat the cancer, and although many of them show success pre-clinically, they fail clinically. It, therefore, becomes important to have a clinically relevant model available that can predict the response of the tumor to therapy. This model has been previously validated against resected clinical tumors. Here a simple protocol to grow desmoplastic three-dimensional (3D)-coculture spheroids is described that can naturally generating a robust ECM and do not require any external matrix sources or scaffold to support their growth.
Briefly human pancreatic stellate cells (HPaSteC) and PANC-1 cells are used to prepare a suspension containing the cells in a 1:2 ratio, respectively. The cells are plated in a poly-HEMA coated, 96-well low attachment U-well plate. The plate is centrifuged to allow the cells to form an initial pellet. The plate is stored in the incubator at 37 °C with 5% CO2, and media is replaced every 3 days. Plates can be imaged at designated intervals to measure spheroid volume. Following 14 days of culture, mature desmoplastic spheroids are formed (i.e. average volume of 0.048 + 0.012 mm3 (451 µm x 462.84 µm)) and can be utilized for experimental therapy assessment. Mature ECM components include collagen-I, hyaluronic acid, fibronectin, and laminin.
Introduction
Pancreatic cancer's poor prognosis is associated with a variety of reasons, among which is its lack of easily detectable biomarkers leading to a late detection. Another major reason is the thick stroma surrounding the tissue, which leads to reduced blood supply. The deposition of large amounts of extracellular matrix (ECM), cell-cell interaction, endothelial cells, various immune cells, pericytes, proliferating myofibroblast, and fibroblast population, and the presence of non-neoplastic cells (together constituting the desmoplastic reaction)1, constitute the thick stroma that is responsible for PDAC's chemo and radiotherapeutic resistance2. Cancer and stromal cells have a complex, dynamic, and bidirectional interaction. Although some elements either attenuate or accelerate disease progression, most processes are adaptive during the tumor's development1. This provides an environment rich with growth factors, proangiogenic factors, proteases, and adhesion molecules. These factors promote angiogenesis, cell proliferation, metastasis, and invasion3,4. Together, they are immune and drug-privileged sanctuary for the tumor, resulting in drug resistance.
The desmoplasia is a complex mixture which consists of various ECM proteins, along with immune cells and pancreatic stellate cells (PSC). Together, these tend to form a scaffold for the cells to grow. PSCs are one of the largest components of the stromal compartment5. Their ability to produce enzymes like matrix metalloproteases (MMP), tissue inhibitors of matrix metalloproteases (TIMP) and cancer associated fibroblasts (CAF)6 imply they are likely to play a critical role in development of the desmoplastic reaction. The ECM, cancer-associated fibroblasts (CAF), and vasculature are the cardinal aspects of PDAC. Among CAFs, myofibroblast and inflammatory CAFs are speculated to be involved in active crosstalk responsible for pro-tumor properties7. The more extensive the fibroblastic formations on the tumor, the poorer the prognosis8,9,10.
Monolayer cell culture through established cell lines continues to remain a useful tool for analyzing drug toxicity and is a good starting point for proof of concept and discovery studies. Established cell culture lines, however, lack germline DNA and clinical relatability11. Since they are grown on flat surfaces, they undergo different in vitro selection criteria compared to when they are a part of the tumor, divide abnormally and lose their differentiated phenotype12. Overall, single cell cultures limit tumor heterogeneity and therefore lose clinical relevance. They are unable to accurately represent the complexity of the tumor's microenvironment (for e.g., the ECM). 3D culture can more closely replicate the complex tumor microenvironment.
3D culture was introduced in the 1970's for healthy cells and their neoplastic counterparts13. Several techniques have been used to study the morphology and architecture of malignant tissues through spheroids14. Co-cultures with stromal cells can model TME signals. An upregulation of EMT markers was seen when cells were co-cultured with stellate cells15. PDAC spheroids and their interaction with the stroma can be modelled by co-culturing with ECM components. Co-culturing specifically with PSCs have been reported to produce clinically relevant drug cytotoxicity data16,17,18. PSCs also aid drug resistance by evading apoptosis and stimulating proliferation of cancer cells through various paracrine factors19 and by inducing EMT transition. It, therefore, becomes critical to include the PSCs from an early stage in the criteria used to evaluate the success of a drug or drug delivery system. The PSC's ability to enhance proliferation and support faster growth in combination, compared to pancreatic cancer cells alone, has also been seen in vivo when subcutaneous flank injections of the two cell lines were evaluated in immunocompromised mice20.
The ability of a cell type to interact with ECM components is also critical to consider when growing co-cultured spheroids. BxPC-3 and PANC-1 have been reported to have equal affinities in binding to collagen. The two cell lines also bind equivalently to laminin, although there have been reports that BxPC-3 binds better21,22,23,24,25. In terms of migration, Stahle et al.26 demonstrated a 5x faster motility for PANC-1 cells as compared to BxPC-3. PANC-1 cells were also reported to migrate primarily as single cells, whereas BxPC-3 cells migrate as a tightly packed sheet. The choice of the cells also affects the size of the tumor25. BxPC-3 tumors were shown to be larger27,28 than those obtained from PANC-1, whereas one study demonstrated the opposite29 case. Despite their differences in size and motility, both cells have been reported to need long periods of latency to form tumors in mice. This duration can be especially long for BxPC-3 ranging from 4 weeks to 4 months25. However, there is also literature where BxPC-328 or BxPC-3 cancer stem cells30 have formed visible tumors quicker, implying there could be variation seen in tumor growth durations. The durations stated here should, therefore, only serve as an initial guideline for tumor growth rates.
BxPC-3 cells form spheroids with loose cells on the surface and dense cores, whereas PANC-1 cells have been reported to form both porous but robust spheroids31 as well as compact spheroids. PANC-1 cells have also been reported to be less differentiated and more aggressive32. Keeping the aggressive nature32 at the forefront, combined with the PANC-1 cells' higher motility, ability to form compact spheroids, and ability to interact with ECM components, PANC-1 cells were chosen for spheroid studies.
In the last few years, spheroid culture has seen a lot of success in demonstrating an advantage in its clinical relevancy compared to two-dimensional (2D) cultures. Its relevance has been leveraged in using this technique as a substitute to animal studies and to better understand the tumors' biology. The clinical relevance of spheroids, especially when co-cultured with PSC's has enabled their use to study various functions of the spheroid such as stiffness33, expression of TGF-β34,35,36,37,38, E-cadherin, F-actin18,34,36,37, α-SMA34,35,37,38, lactate dehydrogenase (LDHA)32, HIF-1α35,39, drug resistance16,37,40, cell migration41, cell invasion37, fibrosis35, radiation resistance42, phenotypical changes18, heterogeneity36, cellular levels of interactions39 and demonstrate ECM components37,38,39. Many of the protocols that were used to obtain the data described rely on Matrigel, the hanging drop method, printed molds, or other scaffolds to help support spheroid and ECM growth. The studies also usually involve the use of either non-human fibroblastic cells or freshly isolated stellate cells from patients. While using stellate cells is critical for the tumors to resemble in-vivo conditions, the inter-patient variability associated with fresh extractions makes these studies difficult to replicate.
This protocol aims to demonstrate a model that is easy to develop, reproducible, clinically relevant, and free of scaffolding, thereby relying exclusively on the co-cultures' abilities to naturally generate the ECM. To do this, a simple co-culture method involving a mix of PANC-1 cells (due to their natural tendency to migrate as single cells) along with human pancreatic stellate cells (HPaSteC) was chosen, due to their ability to behave like stem cells and be highly drug-resistant. Using the studies by Durymanov et al.38as a baseline, the protocol detailed below was established after further optimizing parameters such as cell ratios and durations between media changes. The spheroids resulting from this protocol can be used as a model system for new drug candidate evaluation40.
Additionally, for users not familiar with the spheroid culture, the work Peirsman et al.43discussing the development of the MISpheroID knowledgebase may be helpful. It establishes some minimum information guidelines that could help cope with heterogeneity between lab protocols. Although with some limitations, the work demonstrated that the choice of culture media, cell lines, spheroid formation method, and the final spheroid size are critical in determining the phenotypic properties of spheroids.
Protocol
1. 2D cell culture
- Grow PANC-1 cells in Dulbecco's Modified Eagle Medium (DMEM), supplemented with 10% fetal bovine serum (FBS) under sterile conditions. Grow up to 70%-80% confluency before passages, and do not use beyond the 20th passage. Refer to the process described in step 4.2.1.
NOTE: As a reference point, 1 x 106 cells in 20 mL of media need about 2-3 days to reach 70-80% confluency. - Grow HPaSteC cells in stellate cell media supplemented with 2% FBS, 1% PenStrep, and 1% Stellate Cell Growth Supplement (SteCGS) using the kit supplied by the manufacturer under sterile conditions. Grow according to instructions from the manufacturer (with some modifications) as shown in step 4.2.2 in a Poly-L-Lysine coated flask.
- Skip the FBS neutralization step during trypsinization from the manufacturer's protocol since trypsin neutralization solution (TNS) is used. Neutralize the cell suspension with an overall volume of 10 mL of TNS as described in step 4.2.2.2.
NOTE: As a reference point, 0.5 x 106 cells and 1 x 106 cells in 20 mL of media need 3 days and 2 days, respectively, to attain 90% confluency. - Harvest cells at 90% confluency. Do not use cells beyond Passage 7.
- Skip the FBS neutralization step during trypsinization from the manufacturer's protocol since trypsin neutralization solution (TNS) is used. Neutralize the cell suspension with an overall volume of 10 mL of TNS as described in step 4.2.2.2.
- Maintain cells at 37 °C, with 5% CO2, in sterile incubators with relative humidity at 90%-95%. Perform all cell culture studies in a T-75 flask.
2. Poly(2 -hydroxyethyl methacrylate (poly-HEMA) solution coating for 96 well plate
- Prepare poly-HEMA solution at 5 mg/mL using 95% ethanol by allowing it to be mixed overnight using a heated stirrer at 37 °C. (e.g., 500 mL of solution needs 2.5 g of poly-HEMA)
- Mark the start volume location before adding the stirrer. Use 95% ethanol to make up for any loss in the solution the next day.
- Filter the final solution in a sterile hood using a 0.22-µm filter and store it in the fridge at 4 °C.
NOTE: Poly-HEMA is used to increase the hydrophobicity of a surface, which serves as a deterrent for cells to attach. As this study requires the cells not to attach to the wells and grow as a monolayer, poly-HEMA is used as an additional deterrent to the natural low attachment feature of the plates, thereby making them ultra-low attachment plates. - Add 50 µL of the cold solution to each well of a 96-well round polystyrene bottom microwell plate inside a cell culture hood to coat the plate.
- Leave the wells with the lid on in a hot air oven at 37 °C for 3 days to ensure the plates are completely dry.
- UV sterilize the plates for 30 min in the cell culture hood prior to cell seeding. Store in a tightly closed zip lock for long-term storage and sterilize before use.
3. 2D cell culture planning
- Time the experiment so that PANC-1 cells are available at 70%-80% confluency on the same day the HPaSteC cells reach 90%.
NOTE: Vials containing about 1 million cells of either PANC-1 or HPaSteC, when raised from liquid nitrogen on the same day, with some variation, require 8 days of PANC-1 culture and 6-7 days of HPaSteC culture to have both cell lines ready on the same day.
4. 3D culture growth
- Refer to the overview of the entire process in Figure 1 before starting the process.
CAUTION: Both PANC-1 and HPaSteC are of biological origin. Handle PANC-1 (cancerous cell line) with care. - Trypsinzing and counting cells
- Trypsinze and count PANC-1 cells:
- Discard the supernatant and wash the PANC-1 cells with 9 mL of HBSS (3 mL at a time). Discard used reagents in the hood in a 20-25% V/V bleach solution to ensure complete death of living/viable material.
- Trypsinize the cells with 2 mL of trypsin. After nearly 10 min (may need more time), when all the cells are detached, neutralize the suspension with 10 mL of DMEM + 10% FBS. Begin with 3 mL and follow this with subsequent wash steps using 1 mL per wash (7 washes remaining) to ensure maximum collection of trypsinized cells.
- Pool each neutralized aliquot into the same 15 mL tube. The final volume in the tube will be close to 12 mL (~2 mL of trypsin that has been neutralized with 10 mL media).
- Centrifuge the neutralized cell suspension at 700 x g for 2 min and 30 s. Discard the supernatant and resuspend the pellet obtained in 1 mL of DMEM +10% FBS. Take an aliquot from this for cell counting and label the value obtained from this section as "Count A".
- Trypsinze and count HPaSteC cells.
- Discard the supernatant and wash the HPaSteC cells with 9 mL of HBSS (3 mL at a time).
- Trypsinize the cells with 2 mL of trypsin. After nearly 10 min, when all the cells are detached, neutralize the suspension with 10 mL of trypsin neutralization solution. Begin with 3 mL and follow this with subsequent wash steps using 1 mL per wash (7 washes remaining) to ensure maximum collection of trypsinized cells.
- Pool each neutralized aliquot into the same 15 mL tube. The final volume in the tube will be close to 12 mL (~2 mL of trypsin that has been neutralized with 10 mL of neutralization solution).
- Centrifuge the neutralized cell suspension at 700 x g for 2 min and 30 s. Discard the supernatant and resuspend the pellet obtained in 1 mL of the supplemented stellate cell media. Take an aliquot from this for cell counting and label the value obtained from this section as "Count B".
- Trypsinze and count PANC-1 cells:
- Diluting initial cell suspensions
- Pause at this step if needed (not over 0.5 h) for a short while after obtaining either both counts A and B or after trypsinizing and neutralizing both PANC-1 and HPaSteC. Maintain unused culture media at 37 °C and cell suspensions at room temperature (RT; 25 ± 2 °C).
- Use Count A and Count B obtained previously, to take aliquots and make respective dilutions (in separate tubes) so that the final volume is 1 mL (diluent: DMEM + 10% FBS for both vials) and the final count is between 110,000-140,000 cells for each cell type. Once this dilution is made, verify the cell counts for each dilution to give Count C (PANC-1) and Count D (HPaSteC).
- Pause at this step if needed (not over 15-30 min) after obtaining Count C and Count D. Do not stop once the final dilutions are made in step 4.3.3.2; experiment to avoid cell settling. Maintain unused culture media at 37 °C and cell suspensions at RT (25 ± 2 °C).
- Maintain the final number of cells needed per well at HPaSteC: PANC-1: 60:120. Use 110 wells for the calculation to account for excess. Calculate with a base value of 100 µL of cell suspension per well (total suspension volume is 11 mL for 110 wells with HPaSteC: PANC-1: 60:120). Make this suspension in a sterile 50 mL centrifuge tube for ease of mixing.
- Use Count C and Count D, and spike enough cell suspension into a DMEM + 10% FBS solution to have HPaSteC: PANC-1: 60:120 in a final volume of 11 mL (6,600 HPaSteC cells and 13,200 PANC-1 cells in 11 mL). Mix the solution thoroughly using a 1 mL pipette by stirring and pipetting up and down. Avoid froth formation.
- Seeding
- Use a 200 µL or 100 µL pipette to mix the final suspension (stir by moving the pipette tip around combined with pipetting up and down) at each step prior to adding 100 µL of the suspension per well. Add the 100 µL gently along the corner of the well.
- Re-use the same tip for multiple wells unless it falls off. Mix back and forth and count to 10 or 15 (not seconds) between additions to each well for the first half (roughly the first 43 wells) of the plate. Lower the mixing count to 5-10 between each well for the second half (remaining 43 wells) since the suspension volume is lesser and requires less mixing duration.
- Do not use a repeating pipettor since the hydrophobic poly-HEMA coating will cause the suspension to bounce off the plate, leading to uneven distribution.
- Discard any excess suspension after all wells are filled.
- Use a 200 µL or 100 µL pipette to mix the final suspension (stir by moving the pipette tip around combined with pipetting up and down) at each step prior to adding 100 µL of the suspension per well. Add the 100 µL gently along the corner of the well.
- Centrifugation
- Centrifuge the final plate containing the cell suspension to bring all the cells together as a pellet. Carefully wrap the plate with parafilm around the border of the plate to prevent contamination during this step. Post wrapping, centrifuge the plate with a counterbalance at 1000 x g for 2 min.
- Take the plate back into the cell culture hood (use ethanol-sprayed gloves to handle), remove the parafilm, and store the plates in the incubator at 37 °C, with 5% CO2. Do not spray the plate with ethanol-water mix at any point.
- Culture maintenance
- View cells coming together to form spheroids under a light microscope at 4x-5x magnification by day 3. Follow the culture maintenance protocol as described below.
- On day 3, measure out 5-6 mL of DMEM + 10% FBS and add 50 µL of it to each well along the side of the well.
- Do not mix or agitate the media in any way during addition, as this will damage the spheroid or lead to accidental spheroid removal. The final volume per well will be ~150 µL.
- Beyond day 3, refer to Figure 2 to become familiar with the structure of the well and the location of the light reflection (between the cylindrical and curved portion of the well) seen on the media referred to as the halo. Perform operations close to the halo with caution to ensure the spheroids remain undamaged.
- On day 6, measure 10-11 mL of DMEM + 10% FBS. Use a 1 mL pipette to pull out media in bulk from multiple wells by pulling out media until the halo. Do this for the entire plate, followed by media replacement. Collect supernatant in bulk and discard, or discard it as it is pulled out.
- Replace the discarded media with fresh media by adding 100 µL of media along the side of each well. The final volume in the well will be close to 200 µL.
- Do not pull media beyond the halo, as it increases the risk of accidentally pulling out the spheroid.
- On day 10/11, measure 10-11 mL of DMEM + 10% FBS. Use a 1 mL pipette to pull out media in bulk from multiple wells by pulling out media until the halo. Do this for the entire plate, followed by media replacement. Collect supernatant in bulk and discard, or discard it as it is pulled out.
- Replace the discarded media with fresh media by adding 100 µL of media along the side of each well. The final volume in the well will be close to 200 µL.
- On day 3, measure out 5-6 mL of DMEM + 10% FBS and add 50 µL of it to each well along the side of the well.
- View cells coming together to form spheroids under a light microscope at 4x-5x magnification by day 3. Follow the culture maintenance protocol as described below.
- Final day assessment
- Perform drug treatment on the spheroids on day 14. Image the spheroids prior to use using a brightfield inverted microscope under a 4x objective to determine the start volume of the spheroid. Calculate the Volume (V) using the following formula:
V = 0.5 × L × W2 - Follow the equation to calculate spheroid volumes is described above. Here L is the length of the major axis, and W is the width (longest line perpendicular to the major axis). Convert all original units from micrometers to millimeters to obtain a volume in cubic millimeter.
- The start volume in each well on day 14 is between 150-200 µL due to evaporation. For drug treatments, remove media until the halo is reached from each well and replace it with 100 µL of the drug solution at 2x strength, coupled with some gentle mixing (mix media gently back and forth while counting to 2 between each well).
- Use 2x strength solutions to allow the final drug solution to be at 1x and to avoid completely removing old media from the wells, failing which the spheroids may be disturbed. Use the spheroids within 3 days of this time frame.
- Perform drug treatment on the spheroids on day 14. Image the spheroids prior to use using a brightfield inverted microscope under a 4x objective to determine the start volume of the spheroid. Calculate the Volume (V) using the following formula:
- Spheroid collection
- Measure spheroid volumes prior to collection as described in step 4.7.2.
- Collect the spheroids on day 14 or 17, depending on the experiment's needs, by removing media from each well until the halo is reached.
- Use a 1 mL pipette to remove media and collect the supernatant in a 15 mL conical centrifuge tube from multiple wells.
- Once all the wells have media at the halo level, reduce the setting on the 1 mL pipette to between 200-300 µL.
- Align the plate against the background of the hood or dark background (e.g., a tube rack) to see the spheroids settled at the bottom.
- Gently insert the tip near the spheroid (go below the halo) and pipette a small amount of media (e.g., a visual estimate of close to 50 µL) back and forth to disturb the spheroid. Do not put the tip directly over the spheroid, as this can damage its structure.
- Do not pull all the media out of the well at this step. Control the thumb movement firmly on the piston of the pipette.
- Displace media until the spheroid no longer remains at the center and can be seen moving against the background. Pull up enough media to suck out the spheroid and move it to the desired location (e.g., pool it with other spheroids in a well that is part of the same treatment set).
- Discarding waste
- Discard all liquid samples once neutralized with bleach according to protocols from the respective labs' Environment and Health Safety Department. Autoclave and discard all used pipettes and flasks with biohazardous waste.
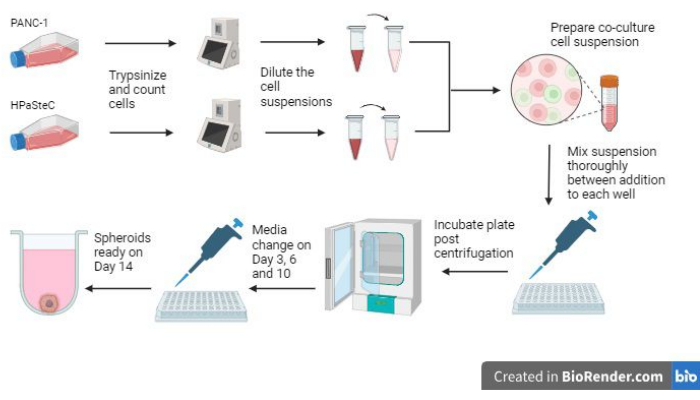
Figure 1: Overview of the process to grow 3D desmoplastic pancreatic cancer spheroids (Generated using BioRender). The figure gives an overview of the basic processes involved; namely, trypsinzing cells, using the initial cell count to make dilute cell suspensions, preparing a co-culture using the diluted cell suspensions, adding cell suspensions to each well, incubating the cultures, performing media maintenance and final spheroid formation as expected on day 14. Please click here to view a larger version of this figure.
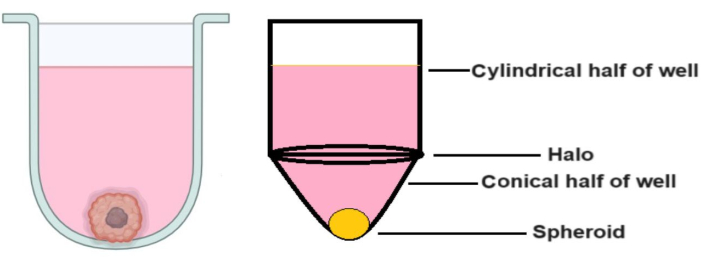
Figure 2: Structure of the U bottom well. The right image is an exaggerated shape to demonstrate the "halo" portion of the well. The figure aims to define where the "halo" portion of the well is as working above the halo is critical to growing the spheroids and avoiding accidental loss. Please click here to view a larger version of this figure.
5. Evaluation of ECM components and confocal microscopy
- Use immunostaining to evaluate the response of the ECM to drug therapy according to the protocol described by Durymanov et al.38.
- Pool the spheroids together and wash twice with 100 µL of PBS. Embed in optimal cutting temperature (OCT) tissue embedding medium, freeze, and maintain at -80 °C.
- Cut the frozen tumor blocks into 10 µm sections, fix the sections in acetone-methanol (1:1) mixture for 15 min, and allow them to air-dry at RT.
- To determine ECM components, immunostain the cryosections with rabbit monoclonal anti-fibronectin primary antibodies, rabbit polyclonal anti-type I collagen antibodies, rabbit polyclonal anti-laminin antibodies, and sheep polyclonal anti-hyaluronic acid antibodies.
- Use goat antirabbit IgG labeled with Alexa Fluor 488 or donkey anti-sheep conjugated with Alexa Fluor 568 as secondary antibodies.
NOTE: Primary and secondary antibodies were diluted at 1:200 and 1:300, respectively. - Acquire images of all spheroid sections using a confocal laser scanning microscope equipped with 20x/0.45 objective lens.
Results
Three of the most critical steps involved in growing the spheroids are the initial cell count, the mixing steps while seeding the spheroids, and performing timely media changes to allow the spheroids to grow (Figure 1). Additionally, being familiar with Figure 2 on media changes after day 3 is critical to allow for effective media changes due to the increased media volume per well. When all these steps are performed according to the directi...
Discussion
The duration and cell ratios chosen to grow the spheroids were based on studies as reported previously38. When attempting to optimize these studies by substituting NIH3T3 cells for HPaSteC cells, spheroid volumes and apoptosis patterns were found to closely resemble the reported optimized parameters (reported for PANC-1: NIH3T3:: 120:12) when PANC-1: HPaSteC ratios were at 120: 60. Although these studies only measure apoptosis until day 14, the protocol described in this process continues to use s...
Disclosures
The authors have nothing to disclose.
Acknowledgements
The work described was supported by the South Dakota Governors' Office of Economic Development, the South Dakota Board of Regents Competitive Research Grant Program (SD-BOR-CRGP), and the Department of Pharmaceutical Sciences at South Dakota State University for their support.
Materials
| Name | Company | Catalog Number | Comments |
| Axio Observer inverted microscope | Carl Zeiss | 0450-354 | |
| Cellometer Auto T4 | Nexcelom Bioscience LLC | Auto-T4 | |
| DMEM, powder, high glucose | Gibco | 12100046 | |
| Donkey anti-sheep conjugated with Alexa Fluor 568 | Abcam | ab175712 | |
| Fetal Bovine Serum | Cytiva | SH3091003HI | |
| Goat antirabbit IgG labeled with Alexa Fluor 488 | Abcam | ab150077 | |
| Hanks Balanced Salt Solution (HBSS) | Gibco | 14175145 | |
| Human Pancreatic Stellate Cells (HPaSteC) | ScienCell | 3830 | |
| Microscope Nikon | Nikon | Eclipse Ts 100 | |
| Nunc 96-Well Polystyrene Round Bottom Microwell Plates | Thermo Scientific | 12-565-331 | |
| Olympus Fluoview FV1200 confocal laser | Olympus | N/A | Discontinued product |
| PANC-1 | ATCC | CRL-1469 | |
| Poly-HEMA | Sigma | P3932 | |
| Rabbit polyclonal anti-laminin antibodies | Abcam | ab11575 | |
| Rabbit polyclonal anti-type I collagen antibodies | Abcam | ab34710 | |
| Sheep polyclonal anti-hyaluronic acid antibodies | Abcam | ab53842 | |
| Stellate cell media complete kit | ScienCell | 5301 | |
| Trypsin | MP Biomedicals, LLC | 153571 | Trypsin solution prepared according to manufacturers protocol and used at 0.25%w/v |
| Trypsin Neutralization Solution (TNS) | ScienCell | 103 |
References
- Hingorani, S. R. Epithelial and stromal co-evolution and complicity in pancreatic cancer. Nat Rev Cancer. 23 (2), 57-77 (2023).
- Laklai, H., et al. Genotype tunes pancreatic ductal adenocarcinoma tissue tension to induce matricellular fibrosis and tumor progression. Nat Med. 22 (5), 497-505 (2016).
- Binker, M. G., Binker-Cosen, M. J., Binker-Cosen, A. A., Cosen-Binker, L. I. Microenvironmental factors and extracellular matrix degradation in pancreatic cancer. J Pancreas. 15 (4), 280-285 (2014).
- Spano, D., Zollo, M. Tumor microenvironment: a main actor in the metastasis process. Clin Exp Metastasis. 29 (4), 381-395 (2012).
- Ware, M. J., et al. Generation of an in vitro 3D PDAC stroma rich spheroid model. Biomaterials. 108, 129-142 (2016).
- Sunami, Y., Häußler, J., Kleeff, J. Cellular heterogeneity of pancreatic stellate cells, mesenchymal stem cells, and cancer-associated fibroblasts in pancreatic cancer. Cancers. 12 (12), 3770 (2020).
- Öhlund, D., et al. Distinct populations of inflammatory fibroblasts and myofibroblasts in pancreatic cancer. J Exp Med. 214 (3), 579-596 (2017).
- Pandol, S., Edderkaoui, M., Gukovsky, I., Lugea, A., Gukovskaya, A. Desmoplasia of pancreatic ductal adenocarcinoma. Clin Gastroenterol Hepatol. 7 (11), S44-S47 (2009).
- Watanabe, I., et al. Advanced pancreatic ductal cancer: fibrotic focus and β-catenin expression correlate with outcome. Pancreas. 26 (4), 326-333 (2003).
- Hu, G., et al. Tumor-infiltrating podoplanin+ fibroblasts predict worse outcome in solid tumors. Cell Physiol Biochem. 51 (3), 1041-1050 (2018).
- Kapałczyńska, M., et al. 2D and 3D cell cultures-a comparison of different types of cancer cell cultures. Arch Med Sci. 14 (4), 910-919 (2018).
- Monberg, M. E., et al. Occult polyclonality of preclinical pancreatic cancer models drives in vitro evolution. Nat Commun. 13 (1), 3652 (2022).
- Emerman, J. T., Pitelka, D. R. Maintenance and induction of morphological differentiation in dissociated mammary epithelium on floating collagen membranes. In Vitro. 13 (5), 316-328 (1977).
- Kelm, J. M., Timmins, N. E., Brown, C. J., Fussenegger, M., Nielsen, L. K. Method for generation of homogeneous multicellular tumor spheroids applicable to a wide variety of cell types. Biotechnol Bioeng. 83 (2), 173-180 (2003).
- Kikuta, K., et al. Pancreatic stellate cells promote epithelial-mesenchymal transition in pancreatic cancer cells. Biochem Biophys Res Commun. 403 (3-4), 380-384 (2010).
- Lee, J. -. H., et al. Microfluidic co-culture of pancreatic tumor spheroids with stellate cells as a novel 3D model for investigation of stroma-mediated cell motility and drug resistance. J Exp Clin Cancer Res. 37 (1), 4 (2018).
- Wong, C. -. W., Han, H. -. W., Tien, Y. -. W., Hsu, S. -. H. Biomaterial substrate-derived compact cellular spheroids mimicking the behavior of pancreatic cancer and microenvironment. Biomaterials. 213, 119202 (2019).
- Liu, X., et al. 3D heterospecies spheroids of pancreatic stroma and cancer cells demonstrate key phenotypes of pancreatic ductal adenocarcinoma. Transl Oncol. 14 (7), 101107 (2021).
- Vonlaufen, A., et al. Pancreatic stellate cells: partners in crime with pancreatic cancer cells. Cancer Res. 68 (7), 2085-2093 (2008).
- Bachem, M. G., et al. Pancreatic carcinoma cells induce fibrosis by stimulating proliferation and matrix synthesis of stellate cells. Gastroenterology. 128 (4), 907-921 (2005).
- Greco, E., et al. Pancreatic cancer cells invasiveness is mainly affected by interleukin-1β not by transforming growth factor-β1. Int J Biol Markers. 20 (4), 235-241 (2005).
- Arao, S., Masumoto, A., Otsuki, M. β1 integrins play an essential role in adhesion and invasion of pancreatic carcinoma cells. Pancreas. 20 (2), 129-137 (2000).
- Sawai, H., Yamamoto, M., Okada, Y., Sato, M., Akamo, Y., Takeyama, H., Manabe, T. Alteration of integrins by Interleukin-1alpha in human pancreatic cancer cells. Pancreas. 23 (4), 399-405 (2001).
- Chen, J., et al. Expression and function of the epidermal growth factor receptor in physiology and disease. Physiol Rev. 96 (3), 1025-1069 (2016).
- Deer, E. L., et al. Phenotype and genotype of pancreatic cancer cell lines. Pancreas. 39 (4), 425 (2010).
- Stahle, M., et al. Mechanisms in LPA-induced tumor cell migration: critical role of phosphorylated ERK. J Cell Sci. 116, 3835-3846 (2003).
- Aubert, M., et al. Decrease of human pancreatic cancer cell tumorigenicity by α1, 3galactosyltransferase gene transfer. Int J Cancer. 107 (6), 910-918 (2003).
- Miknyoczki, S. J., Chang, H., Klein-Szanto, A., Dionne, C. A., Ruggeri, B. A. The Trk tyrosine kinase inhibitor CEP-701 (KT-5555) exhibits significant antitumor efficacy in preclinical xenograft modelsof human pancreatic ductal adenocarcinoma. Clin Cancer Res. 5 (8), 2205-2212 (1999).
- Fukasawa, M., Korc, M. Vascular endothelial growth factor-trap suppresses tumorigenicity of multiple pancreatic cancer cell lines. Clin Cancer Res. 10 (10), 3327-3332 (2004).
- Hernández-Camarero, P., et al. Pancreatic (pro) enzymes treatment suppresses BXPC-3 pancreatic Cancer Stem Cell subpopulation and impairs tumour engrafting. Sci Rep. 9 (1), 11359 (2019).
- Ware, M. J., et al. Generation of homogenous three-dimensional pancreatic cancer cell spheroids using an improved hanging drop technique. Tissue Eng Part C Methods. 22 (4), 312-321 (2016).
- Longati, P., et al. 3D pancreatic carcinoma spheroids induce a matrix-rich, chemoresistant phenotype offering a better model for drug testing. BMC Cancer. 13, 95 (2013).
- Kpeglo, D., et al. Modeling the mechanical stiffness of pancreatic ductal adenocarcinoma. Matrix Biol Plus. 14, 100109 (2022).
- Jang, S. -. D., et al. Anti-cancer activity profiling of chemotherapeutic agents in 3D co-cultures of pancreatic tumor spheroids with cancer-associated fibroblasts and macrophages. Cancers. 13 (23), 5955 (2021).
- Pednekar, K. P., Heinrich, M. A., van Baarlen, J., Prakash, J. Novel 3D µtissues mimicking the fibrotic stroma in pancreatic cancer to study cellular interactions and stroma-modulating therapeutics. Cancers. 13 (19), 5006 (2021).
- Kim, S. -. K., et al. Phenotypic heterogeneity and plasticity of cancer cell migration in a pancreatic tumor three-dimensional culture model. Cancers. 12 (5), 1305 (2020).
- Hwang, H. J., Oh, M. -. S., Lee, D. W., Kuh, H. -. J. Multiplex quantitative analysis of stroma-mediated cancer cell invasion, matrix remodeling, and drug response in a 3D co-culture model of pancreatic tumor spheroids and stellate cells. J Exp Clin Cancer Res. 38 (1), 258 (2019).
- Durymanov, M., et al. Subcutaneous inoculation of 3D pancreatic cancer spheroids results in development of reproducible stroma-rich tumors. Transl Oncol. 12 (1), 180-189 (2019).
- Giustarini, G., Teng, G., Pavesi, A., Adriani, G. Characterization of 3D heterocellular spheroids of pancreatic ductal adenocarcinoma for the study of cell interactions in the tumor immune microenvironment. Front Oncol. 13, 1156769 (2023).
- Alseud, K., et al. Synthesis and biological activity of 11-oxygenated and heterocyclic estrone analogs in pancreatic cancer monolayers and 3D spheroids. Bioorg Med Chem. , (2024).
- Fitzgerald, A. A., et al. Fibroblast activation protein regulates natural killer cell migration, extravasation and tumor infiltration. bioRxiv. , 429622 (2021).
- Wishart, G., Gupta, P., Schettino, G., Nisbet, A., Velliou, E. 3D tissue models as tools for radiotherapy screening for pancreatic cancer. Br J Radiol. 94 (1120), 20201397 (2021).
- Peirsman, A., et al. MISpheroID: a knowledgebase and transparency tool for minimum information in spheroid identity. Nat Methods. 18 (11), 1294-1303 (2021).
- Durymanov, M., Kroll, C., Permyakova, A., Reineke, J. Role of endocytosis in nanoparticle penetration of 3D pancreatic cancer spheroids. Mol Pharm. 16 (3), 1074-1082 (2019).
Reprints and Permissions
Request permission to reuse the text or figures of this JoVE article
Request PermissionExplore More Articles
This article has been published
Video Coming Soon
Copyright © 2025 MyJoVE Corporation. All rights reserved